Nerves and Radicular Pain (ridiculous pain)
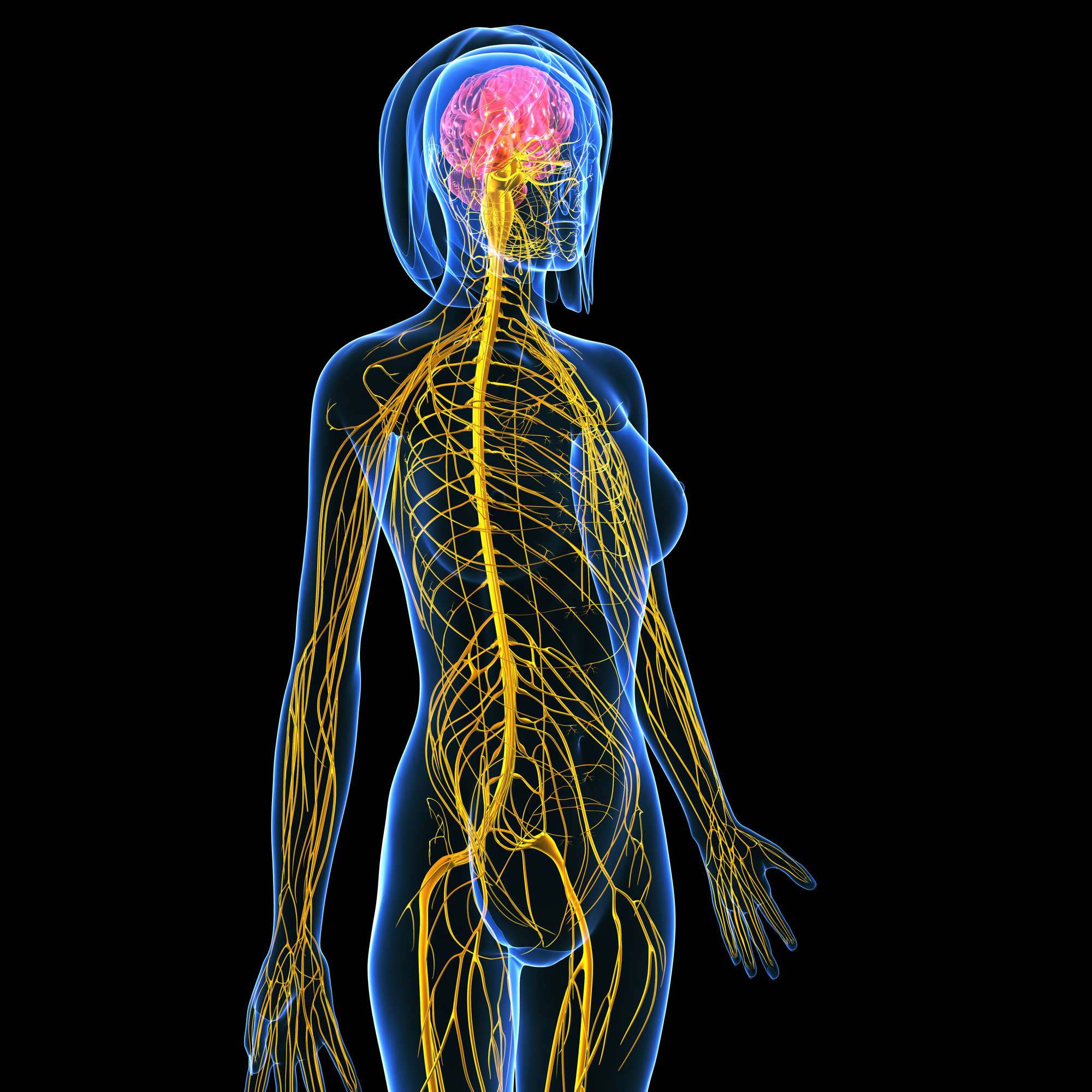
Nerves are NOT invisible
Put simply, I used to think that nerves were microscopic. This was before I knuckled down to five years of study at University. Now I know that every part of the body has a nerve supply and you don’t need a microscope to see them. It all starts from our brain, moves onto our spinal cord and then nerves branch off and travel outward to EVERYTHING and when you put it all together it’s known as the nervous system.
The nervous system is super important
Potentially, I can’t overestimate the importance of the nervous system. We would be a gelatinous blob without it. It manages 100% of everything, 100% of the time and it’s hungry for oxygen and glucose and if it doesn’t get these things it sends danger signals to our brain very quickly so that we can do something about getting them what they need. Normally this will involve fairly basic tasks like moving, moving so we can get something to eat and moving so that we can go somewhere to lay our head and go to sleep.
The nervous system is super sensitive
The 72 kilometres of nerves in our body exist to relay signals/information from bits of our body to the brain or from our pink, squishy brain out to bits of our body. These wonderful information carriers are sensitive to everything; chemicals, touch, movement, they are constantly monitoring every little thing about us. A short distance away from where the nerve exits the spinal cord, there is a very sensitive part that if entrapped or irritated by specific chemicals this may cause increased activity of that nerve. Increased activity means the nerve sends off lots and lots of information to the spinal cord and brain, which you might detect as pain or altered sensation in the skin.
This is what is known as ‘radicular pain’ as it ‘radiates’ through the body, most likely into our arm or leg, along the pathway of a nerve that has exited the spinal cord at your neck or lower down in the spine.
People will present to the clinic with pain into the arm or leg that seems to follow a pathway down a specific area. Radicular pain can present differently for different people. It may be felt as numbness and tingling, or burning pain, or a sharp, jabbing pain, or electric-shock like pain or extreme sensitivity to touch. When a nerve that exits the spinal cord in the low back, commonly radicular pain will be a gnawing, constant pain in their bum.
Who gets radicular pain?
It is estimated that between 13-40% of people will experience radicular pain at some point in their lives. There is a link to age, with the highest number of cases occurring between 40-50 years of age, and genetics may predispose this condition (1).
Is it my job's fault?
Some jobs seem to contribute to the development of radicular pain, such as working in awkward positions where the body is bent or twisted, with your hands above shoulders or when driving for prolonged periods. Equally, sitting a lot is starting to gain momentum as a risk factor for all sorts of conditions, including radicular pain. Smoking also increases the risk of radicular pain, as it alters the metabolic balance within the tissues of the spine (1).
If I have it, what can I do about it?
Most patients with radicular pain experience some improvement within four weeks from the onset of pain (2). The majority of cases resolve spontaneously with a multi-modal approach of pain relief such as anti-inflammatories or opioid based medication (1) and other more conservative measures, like manual and physical therapy or pain education (3). A number of studies supports the theory that a combination of treatments can lead to better outcomes (i.e. less pain) after three months, when compared to patients receiving either medication or physical therapy alone (4).
Can’t you just inject it? Or cut something out?
A 2014 review of research on radicular pain recommends that patients try 4-8 weeks of conservative treatment, before seeking more invasive interventions like spinal injections or surgery (5). It may seem like a long time to wait, especially when pain may cause difficulty sleeping, or reduce our ability to concentrate or enjoy even the most simple things in life.
Osteopathic Intervention
Manual therapy techniques along with exercise based rehabilitation is at least as effective as surgery for radicular pain (5) without the negative side effects. It’s frustrating but learning about what is happening, knowing the prognosis and enjoying even brief episodes of relief can provide hope and keep people focused on the light at the end of the tunnel.
Your osteopath can provide further information on these options. Book online to make a appointment.
(1) Woods, B.I & Hilibrand, A.S. (2015). Cervical radiculopathy: epidemiology, etiology, diagnosis and treatment. Journal of Spinal Disorders & Techniques, 28(5), 251-259
(2) V. J., Lubelski, D., Steinmetz, M. P., Benzel, E. C., & Mroz, T. E. (2014). Optimal Duration of Conservative Management Prior to Surgery for Cervical and Lumbar Radiculopathy: A Literature Review. Global Spine Journal,4(4), 279–286.
(3) Clark, C.L., C.G. Ryan, et al (2011). “Pain neurophysiology education for the management of individuals with chronic low back pain: systematic review and meta-analysis.” Manual Therapy 16 (6): 544-549.
(4) Cohen, S.P., Hayek, S., Semenov, M.A., Pasquina, P.F., White, R.L., Veizi, E., Huang, J.H.Y., Kurihara, C., Zhao, Z. et al. (2014). Epidural steroid injections, conservative treatment, or combination treatment for cervical radicular pain: a multicentre, randomized, comparative-effectiveness study. Anesthesiology, 121, 1045-1055.
(5) Boyles, R., Toy, P., Mellon, J., Hayes, M., & Hammer, B. (2011). Effectiveness of manual physical therapy in the treatment of cervical radiculopathy: a systematic review. The Journal of Manual & Manipulative Therapy, 19(3), 135–142.
This article was a combined effort of Angie Bruce and Cat Burns. Angie was the one who admitted she thought nerves were invisible and Cat provided the bulk of the sensible information and academic references.